Last week’s hiatus was brought to you by My Birthday ™ spent, of course, in the best place on Earth (Brooklyn, NY) with a few of my closest friends and, importantly, no laptop. I appreciate your patience. And, in the words of my RA (shout-out, Tyler): we’re so back.
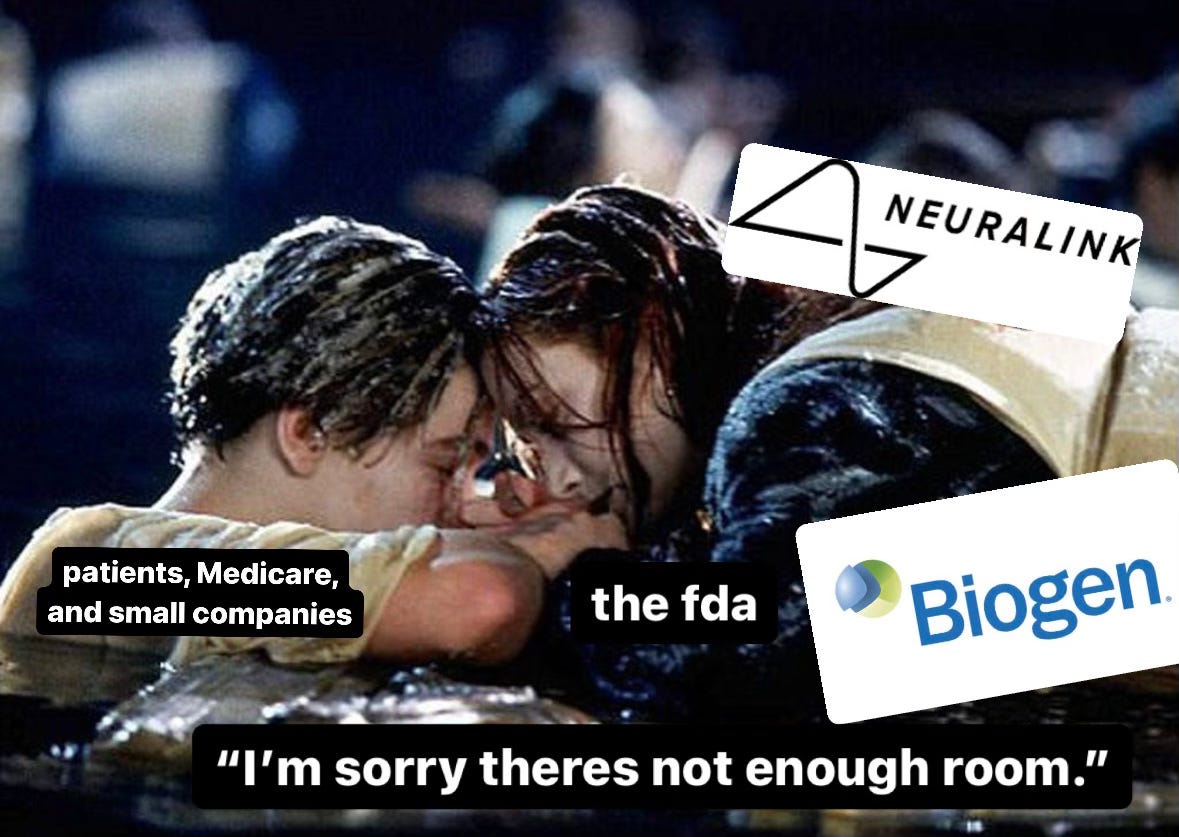
I’m also cheating this week’s Tower post by giving you a taste of Trenches because I think you, Gentle Reader, could use a precedent case in order to fully grasp the heat of the Trenches tea. If you’re familiar with the FDA x Biogen Collab (read: scandal), feel free to skip to the next section.
Manning the (Adu)helm
Despite “a lack of evidence of clinical benefit for patients at disease stages outside of the clinical trials and an unknown safety profile” for Biogen’s Alzheimer’s drug, Aduhelm (aducanumab), the FDA accelerated its approval to market. It was, in fact, internal alarm bells that sounded first, indicating widespread agency consensus that there was insufficient evidence of Aduhelm’s efficacy to grant it any approval—let alone accelerated approval. Apparently, the good researchers of the FDA are helpless in the face of higher-up corporate greed (shocker!) and the $56,000 per year blockbuster promise by Biogen to “establish Aduhelm as one of the top pharmaceutical launches of all time,” beat out responsible clinical sense (I repeat: shocker!).
Over a one-year period beginning in July 2019, the FDA and Biogen exchanged at least 115 meetings, calls, and countless emails. The exact number of these exchanges is unknown because, in direct contradiction to the FDA’s own protocol, no one really kept track of the number of engagements between Biogen and the Agency, and many of them were relatively informal. They also collaborated on a joint document for review by the Peripheral and Central Nervous System Drugs Advisory Committee in November 2020, ahead of Aduhelm’s approval. This collaboration gave Biogen advance notice of the Committee’s likely responses and provided the company with direct guidance, including draft wording, from the Agency itself. Not to mention that, at some arbitrary point in the review process, the FDA pivoted its consideration of Aduhelm from a traditional 9-month review process to an accelerated THREE-WEEK APPROVAL!!!
Bottom line: it’s unethical for the federal agency in charge of reviewing the safety and efficacy of drugs to climb into bed with a high-power drug manufacturer. Duh?!?!
The Wellness-Consumption Paradigm
Unfortunately, the American healthcare industry is—like most American industries—a titanic* capitalist endeavour. Despite the US spending nearly twice as much of its GDP on healthcare as any other OECD country, it remains the only high-income country that doesn’t guarantee healthcare coverage, while maintaining a life expectancy three years lower than the OECD average. There are a number of reasons contributing to this inflated spending: two of them being treatment intensity (e.g., the number of tests, procedures, and treatments that we run per patient) and pharmaceutical expenditure (see: Aduhelm). One day, I will write a manifesto on healthcare system expenditure, but today is not that day. Until then, might I recommend An American Sickness by Elisabeth Rosenthal.
* Titanic, in this case, means “of exceptional strength, size, or power,” not like the ship. Although, arguably (or maybe, prophetically) also like the ship.
Overspending on health doesn’t end in the hospital: “being well” is an increasingly consumerist enterprise, and the lines between medical advice and market power are growing increasingly blurred. Ask any Brit to describe the dystopian experience of watching American pharmaceutical advertisements pop up in the middle of your Netflix show (hi, Nexplanon!), and you’ll see how differently we treat the healthcare industry here…it is, after all, an industry.
Speaking of Brits! If you want to read some really kick-ass work about the 21st-century healthcare model, I leave you to the brilliant Jess Morley, who can do this subject far more justice than I. Nevertheless, I do want to introduce you to the concept of wellness as a perpetually unreachable state over which the US healthcare industry will continue to profit. Once upon a time, you were sick, and then you got treatment, and then you got better. Today—in the age of TikTok psychology, buccal fat removal, and Ozempic—you’ve always got room for improvement. There is always some way to get better, well-er, and hotter…if you’ve got the pockets.
For neurological disorders like Alzheimer’s, breakthrough treatment, though costly, can be life-saving. If we choose to give Biogen the benefit of the doubt, one could argue that any evidence of efficacy justified a push to market—though whether a $56,000-and-three-week push to market was justified is another story. However, the development of breakthrough pharmaceutical products must now compete with modern technological advancements, like medical devices such as brain-computer interfaces (BCIs), which offer new avenues of therapeutic intervention. Move aside, drugs! You’re not the only player in the neuro market anymore.
Not only do BCIs introduce different physiological mechanisms to treat stubborn disorders (e.g., those disorders whose neurological pathways have challenged direct pharmaceutical intervention, like Alzheimer’s and Parkinson’s), but they’re cool, which means they’re marketable. And, in an era of medical marketability, image matters! First of all, you can sell a BCI for way more than $56,000. And, someday, you’ll probably also be able to sell it to people without Alzheimer’s—people who just want to play video games with their brains, for example.
I’ve given you Biogen as an introduction to federal-agency-cross-high-power-manufacturer-collusion so that we can chat about my best friend, Elon, in great detail later.
Trenches Preview
We discuss the potential implications of the FDA’s breakthrough device designation given to Elon Musk’s “Blindsight,” in the wake of Neuralink safety concerns.